Selective Mutism Speech Therapy and Treatment for Children
Selective mutism is a complex anxiety disorder that is characterized by a child’s consistent failure to speak in specific social situations in which there is an expectation for speaking (e.g., at school), despite speaking in other situations (e.g., at home).
As this is primarily an anxiety disorder, treatment for selective mutism should be conducted by a full team that includes a mental health provider along with the speech-language pathologist, the child’s caregivers, and the child’s teachers. This kit should be completed with that full team.
Listen to the Podcast on Selective Mutism Treatment:
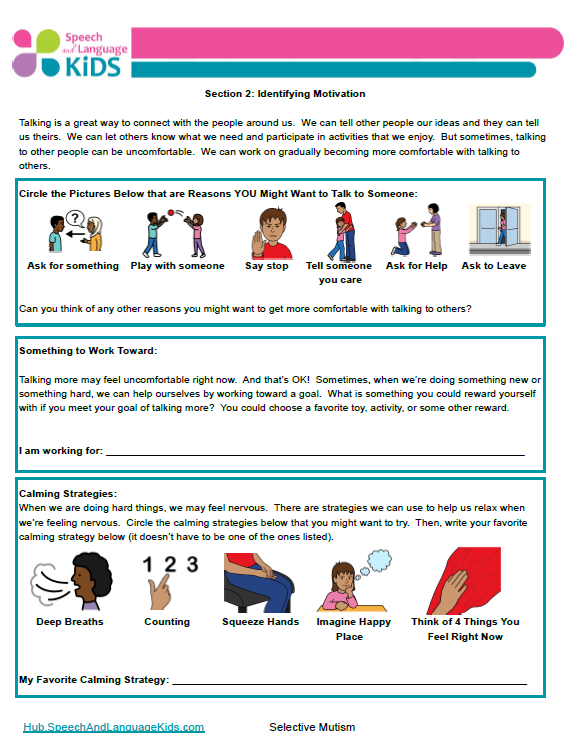
Sample IEP Goal for Selective Mutism
By the end of the IEP cycle, Client will increase spoken communication in the classroom by achieving at least a 4 out of 5 on the following rubric scale as reported by her classroom teacher:
Rubric Scale: Over the past two weeks in the classroom, the student…
1 = Did not speak or communicate in other ways (pointing, gesturing, making sounds)
2 = Did not speak but did communicate in other ways (pointing, gesturing, making sounds)
3 = Spoke every once in a while and also communicated in other ways
4 = Sometimes spoke to participate in school/social activities, but not often
5 = Spoke frequently in the classroom, enough to participate in many school and social activities
Sample Benchmark Goals for Selective Mutism
-
Environmental Modifications: A variety of environmental modifications will be made to increase the client’s sense of control and self-sufficiency in order to reduce anxiety about speaking situations. These strategies include: increasing predictability of their routine, increasing their sense of control about what happens to them, and increasing their sense of self-sufficiency and independence.
-
Identifying Motivation: Client will work with trusted adults to identify three reasons for them to speak to others and three relaxation techniques that can be used to self-calm during anxious moments. *Note: Client will not be required to speak to participate in these activities. The client will be allowed to identify these strategies with pointing, gesturing, and nodding/shaking head (for yes/no questions) if needed.
-
Gradual Changes: Client will gradually increase their ability to communicate in more challenging situations through strategies such as exposure-based practice, desensitization, and shaping.
4 Components of Treatment for Children Selective Mutism:
In 1996, Holly Harris wrote an article called “Elective Mutism” for the Language, Speech, and Hearing Services in Schools Journal. In this article, she outlined the 4 main components of treatment methods for selective mutism. Although you could just select one component to use as your entire treatment plan, it makes more sense to select multiple components and combine them together based on the needs of the individual child.
Component One: Psychodynamic Treatment Approaches
This first component of treatment is what we would call “psychotherapy” or therapy that is conducted by a psychologist or psychiatrist to address psychological concerns in the child. The speech-language pathologist would not be heavily involved in this type of therapy unless additional communication concerns arose during the treatment. However, the other components of selective mutism treatment can be combined with this component (with appropriate collaboration) to create a balanced and cohesive treatment plan. Since I am not a psychotherapist, I will refrain from commenting any more on this component of treatment.
Component Two: Family Intervention Approaches
Some children experience selective mutism as a result of family conflict and problematic family dynamics. If this is the case, family counseling should be provided to alleviate some of these concerns. Again, this would be done by a counselor and not a speech therapist, but the speech therapist does have an important role in family counseling when it comes to teaching appropriate communication strategies and techniques to families.
Families should be kept informed of strategies that are being used at school or in therapy so they can use those strategies at home or in other settings.
To download my handout for parents and teachers on what selective mutism is and how they can help at home and in the classroom, click the button below:
Component Three: Behavior Modification Approaches
Enter: The Speech Therapist! Ok folks, here’s where we jump in. Behavior modification can be added to a treatment plan as a way for speech therapists to help improve functional communication in the school environment (or other settings if working in private practice). For this we will use our trusty sidekick of “Operant Conditioning”. Remember him? Ok, maybe he’s more of a rusty sidekick. Let’s brush off the ole’ college textbook and refresh our memories on this one.
Operant Conditioning comes from our buddy BF Skinner and is based on the premise that behavior which is reinforced tends to be repeated (i.e. strengthened); behavior which is not reinforced tends to die out-or be extinguished (i.e. weakened). Therefore, Operant Conditioning is simply when we change a child’s behavior by reinforcing desired responses and not reinforcing (or sometimes punishing) non-desired responses. Ok, not so rusty, huh? You probably do this every day, you just don’t think about it in such formal terms.
Stimulus Fading for Selective Mutism:
One type of behavioral modification therapy that has been described in the literature is called “Stimulus Fading”. In this approach, you create an environment that the child will be comfortable communicating in. This may include bringing the parent into the school setting (if the child speaks only with the parent) or taking the therapy to the child’s house (if the child only speaks at the home).
Once the child is comfortable and communicating, you gradually make the communication situation more like your target situation (which is usually communicating in the classroom). You will start by gradually introducing a new person to the room (like a teacher or a peer) by first having them in the room but not participating and slowly have them come closer and closer to the child (over a course of several sessions). Then, you have that person interact with the child through the therapist or parent and then eventually get to the point where that person is interacting with the child directly.
Once the child is communicating with several communication partners, then you move those exact people to a new location. For example, you would move the therapy back to school if it was being done at home or you move from the therapy room to the hallway and gradually move closer to the child’s classroom. This gradual transition helps the child become comfortable communicating with different people and in different settings.
Shaping for Selective Mutism
A second behavior modification technique is called “shaping”. In this approach, the child is reinforced for any attempts at communication, starting with gestures or non-verbal communication and those attempts are gradually shaped to audible speech. Once the child is used to being reinforced for non-verbal communication, the child is encouraged to try mouthing words, then whispering, and eventually speaking. This transition is done gradually and at a pace that the child is comfortable with.
When using the shaping technique, the child is reinforced more heavily for communication attempts that are farther along this continuum. For example, if the child merely points to the M&M, she gets one piece of candy. If she mouths the word, she gets two. If she whispers the word, she gets 3. And if she says the word out loud, she gets a whole handful of candy. Keep in mind that the reinforcement must be motivating to that particular child. You may think that getting super excited and loud and hugging a child would reinforce the behavior but if she has some social anxiety already and doesn’t like that kind of attention, it may actually encourage her not to speak out loud again. Some of these children may just want you to very quietly give them a whole bunch of what they wanted as a reward. Just judge what you think the child will like based on his/her reactions.
Component Four: Drug Treatments
The final treatment approach which has been mentioned in the literature is certain medications that are designed to alleviate anxiety symptoms in children (or adults). Again, this is not my area of expertise so I will not be speaking more on that topic, but I wanted you to know what’s available.
Combining Therapy Methods
A complete therapy program should be designed through collaboration with the child’s family, speech therapist, psychologist/psychiatrist/counselor, and teachers/educators. The components listed above should be combined in any manner that best suits the needs of the individual child. For example, the psychologist could be doing psychotherapy and family counseling while the speech therapist is doing behavior modification at the school.
Download the Handout:
Click the button below to download a handout that will explain what selective mutism is and give suggestions for how to help a child with selective mutism:

About the Author: Carrie Clark, MA CCC-SLP
Hi, I’m Carrie! I’m a speech-language pathologist from Columbia, Missouri, USA. I’ve worked with children and teenagers of all ages in schools, preschools, and even my own private practice. I love digging through the research on speech and language topics and breaking it down into step-by-step plans for my followers.
Connect with Me:
Podcast: Play in new window | Download | Embed
Subscribe: RSS






Very useful article! Great info.
I have worked with some selective mute students. I have seen some nice gains by combining same age peers in therapy, that my student selected. We rotated to include everyone. I also did therapy in the lunch room. When she asked for an ice cream I bought her one. Eventually she was verbal in her room.
Another student was on anti anxiety meds and became much more comfortable and verbal.
That’s great! I’m glad you’ve had some successes!
I haven’t had the pleasure of working with any kids with this condition. What assessments are used to determine if a child is experiencing selective mutism or not? If Psychotherapy is the first step and your school rarely has visits or access to a school psychologist, what should be done?
Since this is actually a psychiatric disorder (with communication manifestations), it’s important for the official diagnosis to come from a mental health professional. School districts are legally obligated to provide whatever services a child with a disability needs and I would guess that having access to a psychologist (even if it’s just occasional visits) may be mandated by law for a child with selected mutism. I’m not confident on that though so I would make sure to look into if I were you.
The handout is an excellent resource for parents! Thank you for compiling the resource.
I’ve just begun working with an adolescent student who has a cognitive impairment and is selectively mute. He has been receiving therapy (from psychologists, SLPs) on and off for about 8 years now (since he was 6, he is now 15) and is also on anti anxiety meds. However, he has made limited gains. He does not speak to anyone outside of his direct family (not to relatives or friends even when they visit him at home), and generally has a very blank affect in school. He’s uses gestures to answer questions in my sessions, but hardly does this in school. Though he agreed to it, combining same age peers in therapy has not helped. Suggestions for what I could do with him in sessions would be great. I’m at a loss of what to do at times as it is very difficult to find activities can engage him.
Wow, that sounds rough! I’ve not had any experience with a mutism that has lasted that long. Perhaps it’s too much of a psychological block to move past in therapy. Have you tried using AAC or allowing the child to communicate in some other means like drawing or writing?
It’s been really rough for him and his parents. AAC/ other forms of communication has been a miss with previous slps and in my sessions. He seems adverse to using it (closes the app/ does not press anything when given the ipad). He writes and draws in sessions as part of drawing activities/ language practice but will not do so for communicating. He’ll answer questions only when given choices to choose from with gesturing (pointing, yes/no), and with lots of encouragement to do so. His mutism is deeply entrenched (began in preschool, diagnosed in primary and intervention began a little late) – the psych has mentioned that the mutism has had minimal negative impacts on his functioning as it has been accommodated for in school/ daily life for so long so there’s very little motivation for him to change now. Definitely one of the hardest cases I’ve come across.
Oh wow that sounds like a tough case! I wish I had some magic words that would help but all I can offer are these general strategies here. Good luck!!
Thanks so much for this info! What would you say for a preschooler who has selective mutism? We don’t have school counselors on our campus. We have school psychologists, but they conduct assessments and don’t do any counseling. How about when providing therapy at school. Would you recommend having parent in the room or wait outside therapy room?
Thanks so much for this info! What would you say for a preschooler who has selective mutism? We don’t have school counselors on our campus. We have school psychologists, but they conduct assessments and don’t do any counseling. When providing therapy at school, would you recommend having parent in the room or wait outside therapy room?
Really wish I could access the handout after reading the reviews. However, it appears to be a dead end link to lead pages. What am I doing wrong ?
Hi there! I’m sorry you didn’t receive your free download. We’ve just emailed it over to you. If you are missing any other downloads, please email us at speechandlanguagekids@gmail.com and we’d be more than happy to help!
Hi there! I was sadly unable to get the download for the selective mutism handout. Can you help? Thanks!
Hi, Laurie- Please check your email when you get the chance. We sent over the requested resource.
Can I also access the selective mutism handout? The link does not take you to it.
Hi, Dixie! We have emailed you a copy of the requested handout. Please be in touch shall you need anything further.
very nice post